In June 2015, Jeffrey Thelen’s parents noticed their son was experiencing problems with his memory. In the subsequent years, he would get lost driving to his childhood home, forget his cat had died, and fail to recognize his brother and sister.
His parents wondered: Was electroconvulsive therapy to blame? Thelen had been regularly receiving the treatment to help with symptoms of severe depression, which he’d struggled with since high school. At 34 years old, he had tried medications, but hadn’t had a therapy plan. His primary care physician referred him to get an evaluation for ECT, which was then prescribed by a psychiatrist.
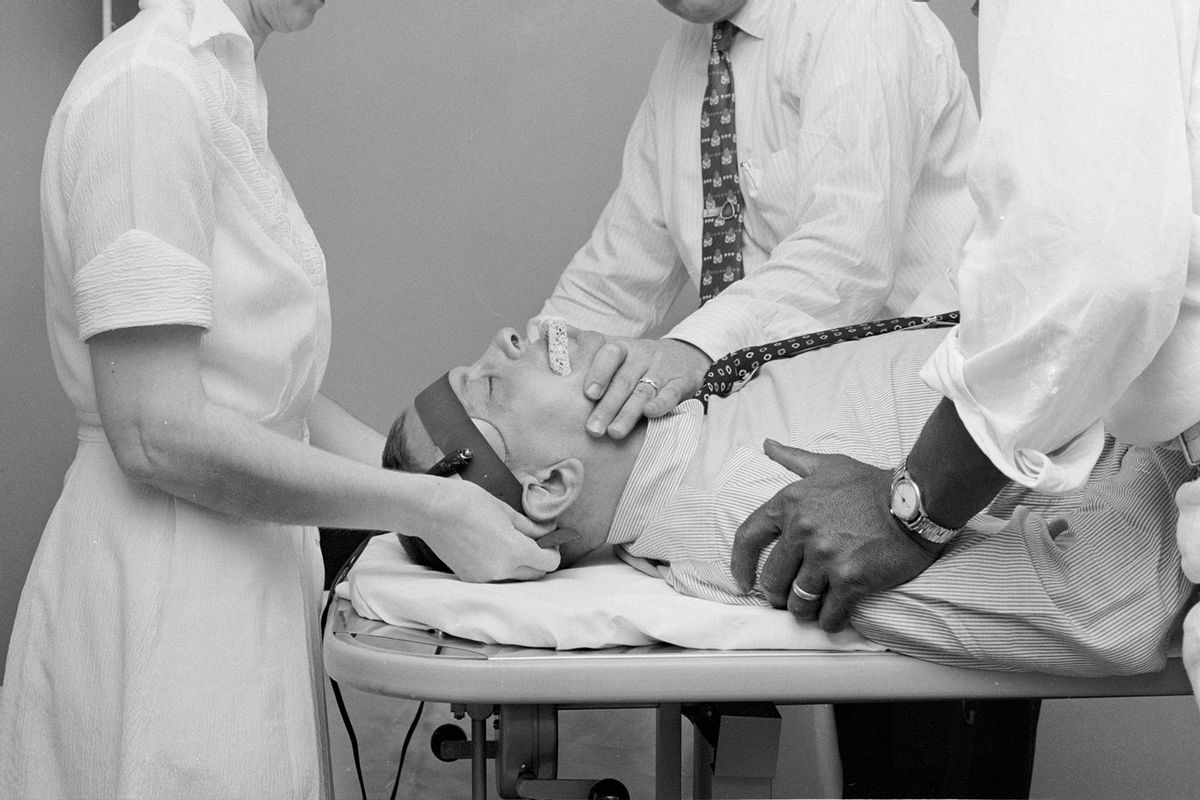
Electroconvulsive therapy has been used to treat various mental illnesses since the late 1930s. The technique, which involves passing electrical currents through the brain to trigger a short seizure, has always had a somewhat torturous reputation. Yet it’s still in use, in a modified form of its original version. According to one commonly cited statistic, 100,000 Americans receive ECT annually — most often to ease symptoms of severe depression or bipolar disorder — although exact demographic data is scarce.
According to one commonly cited statistic, 100,000 Americans receive ECT annually — most often to ease symptoms of severe depression or bipolar disorder.
For Thelen, the treatment appeared to relieve his depression symptoms somewhat, but he reported new headaches and concentration issues, in addition to the memory loss. Those claims are central to a lawsuit Thelen filed in 2020 against Somatics, LLC and Elektrika, Inc., manufacturers and suppliers of ECT devices, alleging that the companies failed to disclose — and even intentionally hid — risks associated with ECT, including “brain damage and permanent neurocognitive injuries.”
Thelen’s legal team told Undark that they have since reached a resolution with Elektrika on confidential terms. With regard to Somatics, in June a jury found that the company failed to warn about risks associated with ECT, but could not conclude that there was a legal causation between that and Thelen’s memory loss. The following month, his lawyers filed a motion for a new trial. (In response to a request for comment, Conrad Swartz, one of Somatics’ co-founders, directed Undark to the company’s attorney, Sue Cole. Cole did not respond to multiple emails. Lawyers for Elektrika declined to comment.)
“The verdict here is significant in that a federal jury, a unanimous jury, decided that, yes, Somatics had failed to warn about risks that are known and that we were able to establish at trial,” said Monique Alarcon, one of Thelen’s lawyers.
Although experts agree that ECT can cause temporary memory loss, the scientific evidence as to whether those effects are permanent is far from settled: John Read, a professor of clinical psychology at the University of East London, was retained as an expert witness by Thelen’s legal team. In his deposition, he testified that somewhere between 12 and 55 percent of ECT patients experience long-term memory loss, and that whatever positive effects exist are short-lived. Read’s view, however, is not shared by all scientists.
While the public perception of ECT — colloquially known as “shock therapy” — has largely been negative, many experts in the field view ECT as a safe and effective tool to help people who are struggling and haven’t found relief from other treatments. In addition to being used to treat depression and bipolar disorder, ECT is also used for schizophrenia, catatonia, and, more recently, self-injury in people with autism, among other conditions.
But even among proponents, there’s little consensus as to what mechanism underlies ECT’s therapeutic effect. And as electroconvulsive therapy is in its 85th year of use, definitive answers continue to elude scientists — and patients.
Understanding how ECT works could offer important clues about the nature of psychiatric illness.
Some researchers say the treatment helps ease depression and other psychological symptoms by promoting the growth of new neurons and neurological pathways. Others have theorized that ECT could impact a patient’s mood by triggering the release of certain hormones. And still others wonder if understanding how it works even matters.
“When I shut down this computer and I reboot it, I turn it back on and it works,” said Michael Alan Taylor, a retired neuropsychiatrist who studied ECT for years. “I know as much about the mechanism of that as I do about ECT. Which is zero.”
Still, understanding how ECT works could offer important clues about the nature of psychiatric illness, said Charles Kellner, an adjunct professor of psychiatry at the Medical University of South Carolina. “The problem is that the brain is a very complicated organ, and ECT changes many things in the brain,” he said. Teasing out which of those changes ease symptoms of depression, for example, will take years, he added: “The good news is that once that is figured out, then we may be able to figure out what’s causing psychiatric illness.”
The idea that seizures might offer some therapeutic potential started to gain ground in the 1930s. Ladislas Meduna, a young neuropathologist from Budapest, had studied the brains of epileptic and schizophrenic patients under a microscope, and observed that epileptic brains featured too many glial cells — which are often referred to as the “glue” of the nervous system and are thought to help facilitate communication between neurons, among other critical functions. Those of schizophrenic patients, on the other hand, featured too few.
Seeing that stark difference led Meduna to theorize that glial cells could have something to do with mental health, and that a seizure might help ease schizophrenic symptoms, including catatonia. To test his theory, Meduna chemically induced a convulsion in a catatonic patient. Several sessions later, the treatment seemed to be a success. For the first time in four years, the patient “got out of bed, began to talk, requested breakfast, dressed himself without any help, was interested in everything around him, and asked how long he had been in the hospital,” wrote Meduna in an autobiography published posthumously. “When we told him that he had spent four years, he did not believe it.”
Meanwhile, in Rome, Italian neurologist Ugo Cerletti had been researching epilepsy by electrically inducing seizures in dogs. He learned of Meduna’s findings but speculated that electricity might be a safer way to induce a seizure compared to the chemical agents Meduna had used.
Cerletti, along with his assistant Lucino Bini and others, administered ECT for the first time in April 1938 to a patient with schizophrenia. After more than 10 sessions, the patient was discharged and Cerletti reported his symptoms resolved, though, according to his wife, they returned two years later.
In spite of those potential side effects, ECT was seen as a gateway towards a prompt recovery at a time when the field hadn’t yet invented key psychoactive drugs.
The treatment wasn’t for the fainthearted, even among its proponents. Max Fink, a neuropsychiatrist and fervent advocate of using convulsive therapies where appropriate, wrote in an unpublished autobiography about witnessing his first ECT treatment in 1952: “As the currents were applied, the neck and back arched, the body became rigid, followed by rhythmic muscle movements and breath holding,” he recalled. “The patient became cyanotic with blue lips, movements stopped, the muscles relaxed, deep breathing followed, cyanosis waned, and color returned to the lips as the patient was moved to a recovery room.” At first, the neuropsychiatrist was “jarred” by the sight of a grand mal seizure. In his training, he had been told repeatedly that convulsions were to be avoided as they could cause fractures and lethal injuries.
In spite of those potential side effects, ECT was seen as a gateway towards a prompt recovery at a time when the field hadn’t yet invented key psychoactive drugs, such as SSRI antidepressants. But use of the treatment declined in the 1960s and ’70s, when a growing anti-psychiatry movement, along with troubling depictions of the treatment in popular media, contributed to a negative public perception. The 1975 film “One Flew Over The Cuckoo’s Nest” is among the most infamous portrayals, depicting ECT as a violent punishment to subdue an unruly patient.
“There’s no doubt that the stigma is what has kept it from wider use,” said Harold Sackeim, a professor of psychiatry and radiology at Columbia University and the former chief of biological psychiatry at New York State Psychiatric Institute. Sackeim, a long-time researcher of ECT, is a proponent of the treatment. “Most people say that it really did help them,” he added. “You can convince people, but it’s a hard sell.”
Anti-ECT activists have been vocal about what they see as the negative side effects. Fink, who has researched the treatment for 70 years, vividly remembers a lecture he gave in the early 1990s: A woman who had previously undergone ECT accused him of failing to recognize the terrible side effects she said the treatment had on her memory and cognitive capacities. She then handed him a frying pan filled with an animal’s brains on a bed of dollar bills.
Many of ECT’s core principles remain unchanged from when it was first introduced. But the treatment has evolved to improve effectiveness, reduce side effects, and protect patient safety. For example, ECT was originally administered without anesthesia or muscle relaxants, which made vertebrae fractures more likely. Those drugs are now considered part of standard care. Research has also been conducted to determine optimal electrode placement. Positioning electrodes on just one side of the head, rather than both sides, is increasingly recommended for less severe cases.
A typical ECT patient today undergoes a total of six to 12 treatments over three to six weeks. But some patients require regular sessions for a longer period of time. Thelen, for example, had more than 90 ECT sessions over the course of two years, according to court documents. This rarely but increasingly practiced method is called “maintenance” ECT or “continuation” ECT.
In 2018, ECT devices were reclassified by the Food and Drug Administration, which allowed the treatment to be more accessible to adolescents suffering from catatonia and major depressive episodes. ECT practitioners increasingly adapt the treatment according to the patient’s age, sex, electrode placement, or seizure threshold — the amount of electricity needed to trigger a seizure — so that the dose is as low as possible to reduce side effects — yet still effective.
George Kirov, a professor of psychiatry at Cardiff University in Wales, acknowledged that developments to reduce side effects have been a positive advance in the field.
As researchers debate ECT’s effectiveness — and patients wonder about side effects — the field still lacks consensus about the mechanism by which it works. There are several theories, in part because ECT has been found to elicit so many changes in the brain that it can be difficult to pinpoint exactly which are affecting behavior. Various studies have found it can change everything from how blood moves through the brain, to how genes related to brain function turn on and off, to how parts of the brain communicate.
“It is really a complex effect,” said Maryna Polyakova, a postdoctoral researcher at Max Planck Institute for Human Cognitive and Brain Sciences in Germany. “This is the reason why we cannot explain it so easily.”
Despite the evidence, many experts feel the neuroendocrine approach doesn’t fully explain ECT’s benefits.
Still, scientists have tried. One leading theory proposes that ECT changes brain chemistry: Electrical signals trigger the release of certain neurotransmitters, chemicals that help brain cells communicate, such as dopamine and serotonin, which can then help stabilize mood. Other theories say that ECT may help foster the growth of new neurons — a process that scientists still debate — or can help create and maintain connections between neurons. Because those effects are difficult to observe in living patients, most studies are done on human brains post-mortem — as Meduna did in the early days of convulsive therapies — or on rodents.
Another idea is the “neuroendocrine hypothesis,” which was first proposed in the 1980s by Fink and the late Jan-Otto Ottosson, a Swedish psychiatrist and historian of ECT. The duo looked at a circuit in the brain called the HPA, or hypothalamic-pituitary-adrenal, axis, which helps govern the body’s response to stress. For patients with depression and other severe mental illnesses, the HPA axis often doesn’t function as it should. Fink and Ottosson theorized that ECT-induced seizures might improve mood by triggering the release of various hormones. Although it has lost some of its initial appeal, there are studies to support it.
But Kellner, who has collaborated with Fink, said that despite the evidence, many experts feel the neuroendocrine approach doesn’t fully explain ECT’s benefits. “ECT does change neuroendocrine functions tremendously, and that’s certainly a part of it. But that may be a downstream thing, rather than the main initial part of why ECT works,” Kellner said. Changes to the HPA axis are “certainly an integral and important part. Whether or not that’s the big driver? I don’t think anybody knows.”
Most researchers have long thought that ECT’s therapeutic potential comes from the seizure itself, but others suggest what really matters is how the brain protects and repairs itself after the seizure.
Indeed, it became apparent that as patients received ECT, the amount of electrical current required to induce a seizure would increase over time, so Sackeim and his colleagues proposed what’s known as the anticonvulsant theory — the idea that ECT gradually improves the brain’s capacity to prevent seizures by inhibiting the region of the brain that is hyperactive in patients with depression. “The only reason why we’re triggering the seizure is to get the brain to stop it,” said Sackeim.
The researchers suggested this might have something to do with the transmission of a neurotransmitter called GABA, which is like the brake system of the brain and allows “the brain to function at the right speed,” said Dirk Dhossche, a former student of Fink and medical director of the child and adolescent unit at Inland Northwest Behavioral Health in Spokane, Washington.
A small 2008 study involved 25 patients with depression, all of whom had lower GABA levels at the start of the experiment compared to healthy patients. The depressed patients went through seven to 12 sessions of ECT. Three days after their last treatment, researchers found their GABA levels had increased significantly.
In recent years, the idea that ECT works by promoting the creation, maintenance and growth of neurons — what’s known as the neurotrophic hypothesis — and by helping boost neural connections — the neuroplasticity hypothesis — has begun to gain ground. “There’s a tremendous amount of neuroimaging research in the last five to 10 years that shows the neurotrophic hypothesis and neuroplasticity hypothesis are probably even more important than the neuroendocrine ones,” Kellner added.
“ECT probably releases important chemicals that support glial cells and enhance their function in some way. But it’s certainly not understood at a fine level yet.”
Some researchers have revisited Meduna’s initial suggestion that the therapeutic effect of seizures had something to do with glial cells, the glue of the nervous system, which seem to play a role in mood disorders. But as Kellner, the professor at the Medical University of South Carolina, pointed out, scientists still don’t have a complete understanding of exactly how glial cells operate.
“We still don’t know what glial cells do,” said Kellner. With renewed interest in their function, he continued, “people are beginning to go back to that very old theory about glial cells and say, you know, ECT probably releases important chemicals that support glial cells and enhance their function in some way. But it’s certainly not understood at a fine level yet.”
“It’s going to take another 10 years to figure that out,” he added.
Still other researchers suggest that there is no single pathway by which ECT works — instead, it could be a combination of these different theories, perhaps with some pathways helping certain disorders more than others. “ECT is actually such a big, big stress for the brain. It’s short term, but it is a very big stress. So it’s not surprising that all the mechanisms which were ongoing just before the shock would be stimulated,” Polyakova said.
“And that’s why,” she continued, “I don’t think there is a single mechanism of action.”
In Jeffrey Thelen’s lawsuit against the ECT device manufacturers and suppliers, the central question is about long-term memory loss, and whether the companies should have done more to warn Thelen, and all ECT patients, of those risks. Thelen was informed by his doctors about losing memories immediately before and after the treatment. “I was okay with that,” he recalled in his deposition.
“Waiting in the waiting room,” he continued, “who cares if you forget that.” But he was unaware that the effect could potentially last much longer. “Thirty-five years compared to 30 minutes, that’s ridiculous,” he said.
Even though the majority of patients do not seem to experience long-term adverse effects, Thelen is not alone in reporting them either. Sarah Price Hancock says she underwent 116 ECT sessions between 2002 and 2009, and is critical of the treatment. “I have no memory of 36 years of my life,” she said.
Loretta Wilson received about 60 treatments starting in 1993, when she was in her 50s. ECT triggered, according to her, significant autobiographical memory loss. “I have no memory of my own wedding,” she said. She says she also doesn’t remember the birth of her children. “I don’t remember their birthdays.”
“Some specific memories may be erased. But you know what I say? So what? You saved the person’s life.”
While memory loss is a documented side effect of ECT, proponents of the treatment claim that it is temporary. “ECT does not harm memory function long term,” said Kellner. However, he did note that, while a person is undergoing treatment, “some specific memories may be erased. But you know what I say? So what? You saved the person’s life,” he said. “And we’re back to that same thing where people don’t understand that these are life-threatening illnesses.”
Fink takes a similar approach: “If a person goes to surgery, and they lose a pint of blood, they lose blood. You have to put new blood in. People who get ECT lose some memory. And then in time it comes back,” he said.
“You can’t do surgery without some blood change,” he continued. “As an example, I use that as an argument, and you can’t give ECT without some memory change.”
Indeed, the debate over ECT often centers on its cost-benefit ratio. In a 2010 literature review on the effectiveness of ECT, Read, the University of East London professor who testified in Thelen’s trial, and co-author Richard Bentall wrote that “the cost-benefit analysis for ECT is so poor that its use cannot be scientifically justified. ” In that review, Read and Bentall examined 60 years of scientific literature on ECT with a primary focus on depression. They found little evidence for improvement during the treatment and none afterwards.
But many researchers stand by the treatment. “Anything you do in medicine is a risk-benefit calculation,” said Kellner. “And the risk benefit calculation for ECT is so far in favor of the benefit that it’s one of the best and safest procedures in all of medicine.”
Part of the issue is that there are still so many unknowns in the study of memory. The brain forms long-term memories through a process called consolidation. If a person is given a random streak of numbers, they will likely not remember it one hour, let alone days, after learning it. But if that streak of numbers is repeated over and over again, the brain conveys this information from short term to long-term memory. Electrical stimuli like ECT prevent the brain from transferring the information, explained James McGaugh, a retired neurobiologist whose research focused on learning and memory.
In the 1990s, a task force for the American Psychiatric Association, a widely recognized authority in the field, published a report with draft guidelines for practitioners to follow. Until then, ECT proponents had argued that the treatment could do no wrong — that it was totally underutilized and had no side effects, only transient ones. “That wasn’t true,” said Sackeim, the Columbia University professor. His research team “showed without a doubt that you can have persistent memory effects, that these things can last forever. But it’s also the most effective treatment that there is. I mean, there can be two truths.”
Sackeim’s team had devised a test intended to assess memory loss post-ECT. They asked people some 300 facts about their lives, ranging from old, new, neutral, positive, and negative memories. “We were able to show, depending on what type of ECT you got, the amount of amnesia immediately after the treatment course, two months after the treatment course, six months after the treatment was different.”
But even though patients usually score well on these kinds of tests, when asked whether ECT hurt their memory, they often report it did. Complicating things further is the fact that people who are treated with ECT, such as Wilson and Hancock, are often on a cocktail of medications, which along with mental illnesses themselves, have documented impacts on memory.
Meanwhile, critics of ECT point to the field’s lack of research studies. In his testimony at Thelen’s trial, Read noted: “The research is very poor. There is very limited research, and the methodology is not good.”
Many researchers argue that ECT should be used as a primary treatment for severe depression.
Kellner disagrees. There is already a large amount of high-quality ECT research, he wrote in an email to Undark. He, however, acknowledges that the field does need more funding. “Compared to studies of heart disease and cancer, the funding has been minuscule, and part of the reason is that there’s no industry to support it. There’s no pharmacology industry to support ECT research,” he said. Among the studies that are conducted, some do involve a small number of patients and lack a placebo group. But Kellner insists that this is not unusual. Looking at studies of any medical procedure, he said, some will have small cohorts while others — including those for ECT — will have very large ones.
Still, many researchers argue that ECT should be used as a primary treatment for severe depression. To this day, some of the most pivotal work done in the U.S. to examine ECT’s impact on such patients with depression has been led by the Consortium for Research in ECT, or CORE, initially conducted by Fink, Kellner and two colleagues, and the Columbia University Consortium. According to the CORE findings, ECT seems to work quicker than medication and should be considered earlier in the course of treatment.
In the neurobehavioral unit at the Kennedy Krieger Institute in Baltimore, Lee Elizabeth Wachtel refers children, teenagers and young adults to be treated with ECT. She believes the proof lies in how many patients ECT has already helped, reflected by numerous published case studies, bolstered by extensive literature from the past 80 years.
Part of Wachtel’s work focuses on catatonia in patients with autism. But she said introducing a controlled study is ethically questionable: “It’s impossible to lead studies because you need two groups of patients: catatonic patients getting ECT and others with the same condition not getting the treatment,” she said. “We know ECT works on catatonia, not giving it for the purpose of a study would be cruel.”
The lack of predictability can be unnerving for prospective patients, many of whom have tried various other treatments with limited to no beneficial effect.
To reduce the cognitive side effects, ECT practitioners have been using less invasive methods that lower risks of cognitive side effects but also remission rates.
Other brain stimulation techniques have been developed as well: Transcranial magnetic stimulation, for instance, “uses magnetic fields to stimulate nerve cells in the brain,” according to the Mayo Clinic, and is less invasive than ECT. Magnetic seizure therapy is another alternative but operates at a significantly higher frequency than TMS so it requires that the patient be anesthetized. Both innovations are representative of the field’s effort to personalize treatments by targeting certain areas of the brain as opposed to overwhelming it with electrical currents.
In the 20th century, experiments of ECT on rodents revolutionized researchers’ understanding of memory. “Electroconvulsive shock studies were critically important in the early stages of understanding the physiological basis of memory in the 1950s, ’60s, and ’70s,” said McGaugh.
The same could be true about the causes of psychiatric illness if researchers can better understand the mystery behind ECT, according to Kellner. “The only people who get ECT are very, very seriously ill, so they represent a much purer biological sample of people with these particular illnesses than are treated by psychotherapy or medication,” he said. “So it’s a subset of much more severely ill people who, by nature, have a more specific genetically transmitted type of the illness. And that’s why ECT is a wonderful platform to look at. Not only how ECT works, but what’s causing psychiatric illness.”
Understanding what causes someone to be sick could lead to a greater personalization of treatments. For patients such as Thelen, who struggled to find an effective treatment for the better part of two decades, this could be life changing.
For many practitioners, ECT is still seen as worth the risk. “I know how to give it so that people are safe, and they get better,” said Michael Alan Taylor, the retired neuropsychiatrist and ECT researcher. “And for me, that’s enough at the moment.”
As for Thelen, his lawyers filed a motion for a new trial.
This story was supported by a grant from the Pulitzer Center.
This article was originally published on Undark. Read the original article.

Read more
about mental health