Statistics reveal rhinoplasties to be the most popular facial plastic surgery procedure, trending upward since 2020, according to the American Academy of Facial Plastic and Reconstructive Surgery (AAFPRS). In addition to its universal appeal across genders and ages, this is also due in part to its dual functional role in restoring nasal breathing. In fact, board-certified plastic surgeon Jason Roostaeian, a rhinoplasty expert and clinical professor at UCLA, estimates that 75 percent of his surgeries include septum repair of a deviated septum, also known as a septoplasty.
As a beauty editor, I have known for years that if I ever opted for a nose-related procedure, Dr. Roostaeian would be my chosen doctor. I love his natural results, which I call a “tidy” aesthetic: nose bridges are straight but never “scooped,” occasionally leaving hints of dorsal character on the bridge; nose tips are always refined and yet never pinched or upturned (once healed). Aesthetically, he takes the overall harmony of the face into consideration while the nose’s structural integrity is prioritized and even improved surgically.
But it was debatable whether the ultra-subtle results I sought would be worth the stress, costs, and risks of surgery: why go through an invasive procedure when post-op swelling would presumably exacerbate my aesthetic concerns for months before resolving them? My exterior concern was that the tip lacked refinement, widening and turning downward when I smiled. Two trusted plastic surgeons, though not rhinoplasty experts, had mused that a “baby rhino” was probably not worth it. Yet as a bonafide wellness fanatic (a Virgo, with four major planets in the Zodiac’s most health-minded house), I was also intrigued about the “two birds, one stone” efficiency of the septo-rhinoplasty, a combined rhinoplasty and septum repair from a deviated septum. I have always had a passion for complementary alternative modalities and integrative health — including a love of breathwork, from the Wim Hof technique to yogic practices.
I did have a deviated septum that I now suspect is linked to complications I dealt with from my severe allergies. By my 30s, I had managed the worst of my symptoms by removing allergens from my life — namely, by giving up horseback riding and limiting exposure to my equine “babies,” Sunny and the now-deceased Hans — but after a miserable bout of COVID-19 while in Italy last August, I revisited the matter. I was again plagued with residual sinus pain and more frequent wake-ups in the night feeling that my nasal pathway was blocked and inflamed. My boyfriend and I had gotten into a fight while I was quarantined abroad in his childhood bedroom, and the rebellious ring of a “revenge rhino” propelled me to book my consultation. (Dr. Roostaeian did not love the term and was quick to lecture me that any surgical procedure should be done only for my own happiness.)
Keep reading to learn about my experience getting my super-subtle, ultra-natural baby rhino procedure with Dr. Roostaeian.
The Process: Choosing Your Surgeon
Opting for any surgery is a highly personal decision, and it is important to take your time researching the procedure and your preferred surgeon. I have had extensive professional opportunities to review surgeons’ rhinoplasties for years. By helping my best friend in her search for a rhinoplasty surgeon (and even attending multiple consultations with her at some of the most renowned surgeons’ offices in California), I had already long-selected Dr. Roostaeian as my preferred rhinoplasty expert. This removed a major stressor from the process.
Understanding the ins and outs of the procedure helped me mentally prepare. Because he is a professor, he took the time to go in depth on its evolution — from the structural rhinoplasties of the 1980s/early 2000s (wherein cartilage was cut away but left the nose lacking in strength), to the structural rhinoplasties that use cartilage grafting to reinforce longevity and strength, to the minimally invasive preservation philosophy that salvages as much of the bridge, soft tissues/ligaments, and cartilages as possible. In my case, the end result would be more aligned with my aesthetic preferences but also structurally stronger than before, facilitating better breathing for the long-term.
Photos are great, but it also really helps to see a surgeon’s work in person. Before I even knew Dr. Roostaeian, I was introduced to a patient of his that was only one week out from surgery. I was so amazed by her beautiful, natural results, and her rapid healing time, that I asked for his information on the spot. Aside from his word-of-mouth repute within the industry, the other reasons I knew he was “the one” for the job were his demonstrated aesthetics, his surgical technique, the consistency of his results, and certain perks to having the surgery at UCLA Health.
What Is a Baby Rhinoplasty?
A baby rhinoplasty can look like many things, but it typically involves the surgeon making minimal changes for a more natural-looking nose job. As for the subtlety of my own procedure, I knew that Dr. Roostaeian’s use of cutting-edge equipment like the ultrasonic piezotome (which minimizes damage to the surrounding tissues and reduces downtime) would afford him the precision needed in a surgery where “every millimeter counts.”
I personally looked for his patient cases where he preserved degrees of the dorsal hump, because I like the character on the bridge of my nose. (Occasionally, he also does this to avoid feminizing the faces of men patients.) Most importantly, even when straight, his bridges are never “scooped” once healed.
Not all baby rhinoplasties are combined with septoplasty, but they can be. You also don’t need to go to a pricy plastic surgeon for the latter, but the benefit of having my surgery at UCLA meant that they submitted my septoplasty directly to my insurance. (As board-certified plastic surgeon Sam Rizk, MD, points out, if you ever consider a rhinoplasty, doing it simultaneous with the septum repair ensures you do not need cartilage later on.) Though unseen, it plays an important medical role, while Dr. Roostaeian’s subsequent aesthetic work protects the longevity of your repair. “The nose is a better filtration system for your breathing, from your nasal hairs to all the mucosal surface area,” he says.
My Baby Rhinoplasty Consultation
At my consultation, we spoke about my concerns and my preferences, and he showed me past patients’ before-and-afters whose cases compared most closely to mine. As mentioned, my concerns ultimately came down to the lack of refinement toward the tip of my nose, which turned downward and appeared to widen when I smiled. Dr. Roostaeian noted that this was caused by a lack of support in the tip creating a contour of light and dark that bothered me. By adding support to the tip with a piece of cartilage from my septum — what is technically a “tipoplasty” — he would be able to strengthen my nose, create a light-contour that created the refined aesthetic I craved, while fortifying the septum repair and ensuring better breathing over the long-term. My cartilage would be maintained, but subtly overlap, to yield symmetrical and result in improved structural integrity.
He would perform this via an open surgery, and because of my deviated septum, a large portion of my surgery would be submitted to insurance. I also knew he would take his time “tinkering” while I was on the table to ensure that the end result met his perfectionistic standards.
The main question was: why go through a lengthy healing time where my swollen nose would temporarily appear less refined than before, particularly when my “before” was not so dire? Well, because my baby rhino would be relatively minimal — my nose would not be broken; he referred to it as more of a “finesse” — his delicate technique was important to me. I felt confident in his demonstrated minimal downtime (thanks to his technique and things like creating his own nasal stents to facilitate drainage and lessen bruising and pressure), so I felt ready to commit.
My Baby Rhino Prep
Five days before surgery, Dr. Roostaeian had me begin applying antibacterial ointment to the insides of my nostrils. I had to discontinue certain supplements, like my fish oil, but incorporated others, like the HealFast Pre-Op Healing Optimization Formula and Post-Op & Injury Formula ($100, originally $120).
As Dr. Roostaeian points out, the surgeon can only control what is happening on the surgical table. After that, the body takes over and the long-term healing process begins. It is up to your decisions to help or hinder this process — and I had every intention to help it. I booked an appointment with naturopathic doctor Nadia Musavvir to create a plan to optimize my recovery. After running everything by Dr. Roostaeian for approval, she helped me with healing supplements like liposomal vitamin C and enteric-coated Bromelain ($16), tips on tweaking my diet to reduce post-op inflammation, and recommended wellness practices to support my recovery. I stocked up my fridge with vegan broths and soups from Erewhon, organic berries to add to my InflammaCore smoothies, and special probiotics to take both while on antibiotics and after getting off of them.
Day of Surgery
On the morning of surgery, I dropped my dog off at her dog sitter and checked in to the L’Ermitage Hotel in Beverly Hills, where I would stay overnight. Then I headed over to UCLA Medical Center.
I was a little nervous but felt better at the hospital. I found the professionalism of medical personnel, whose everyday exposure to these procedures makes them normalized, very comforting. Once in pre-op, a flurry of nurses and health experts took my vitals and asked me questions, running me through what to expect. Then I waited in the bed in my hospital gown under heated blankets, wishing I could drink water and have a snack. When Dr. Roostaeian arrived, he showed me the drawings he had prepared to plan out my surgery. Then the nurses gave me a sedative cocktail, and I was asleep before I even reached the surgical room.
From what I’ve gathered, Dr. Roostaeian created an incision in my columella to get a better look at the inside of my nose (this is what makes it an “open” rhino). He was surprised by the extent of my deviated septum toward the top (or “posterior”) of my nose, which helps to explain my years of improper drainage from my sinuses. As expected, he repaired my septum and used some of its cartilage to build structure behind the tip of my nose — creating a more contoured tip, but also providing the strength that would account for the longevity of my results and improved breathing. For overall harmony, the bridge was lowered a bit from the base, and some cartilage was made to overlap for strength and symmetry. A hint of my dorsal hump was also maintained.

When I woke up, I was in a hospital bed surrounded by Dr. Roostaeian and two of my friends. I had a cast on the outside of my nose with tape creating pressure beneath it. I felt no pain but was very drowsy and wondered if I had had an intense “night sweat” because my hair was wet. (I didn’t — they washed it.) Dr. Roostaeian went over my prescriptions with me, answered a few of my questions, and showed me my before-and-after pictures from the operating table. Then it was time to go.
When we got to the hotel, I had planned to order room service and watch a movie for a girl’s night. No sooner had I changed into Clementine silk pajamas and propped myself up against the monogrammed pillowcase, that I fell asleep. I got up frequently throughout the night to go pee thanks to all the fluids during surgery, but I slept on and off for about 13 hours before checking out in the morning.
Healing Week 1
The most jarring part of the entire process was that I could not focus my eyes when I woke up the next morning. Then Dr. Roostaeian let me know that my problems focusing were from an anti-nausea patch behind my ear. Once I removed it, things quickly went back to normal.
When I got back home, an extensive regimen of antibiotics, anti-inflammatories, and healing supplements kept me occupied. I had been told by surgeons in the past that rhinoplasty recovery was not painful, but I didn’t believe them. The fact is, it wasn’t. I was bruised and puffy, but I didn’t even take Tylenol during my recovery. Only the unbearable congestion was uncomfortable; I didn’t know it yet, but there were giant stents up the inside of my nose to support my septum while it healed.
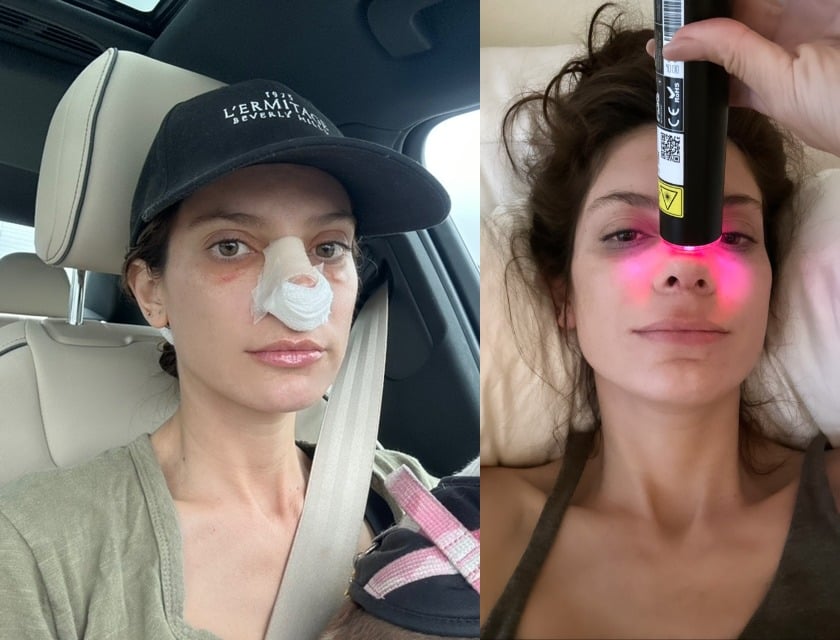
I kept all pressure off my nose, but I used my favorite at-home device, the Lyma Laser ($2,695), to reduce inflammation and promote healing on the exposed tip. I knew the tip would take the longest to heal, and while inflamed, it would appear to be rotated upward, which I dreaded. This was my main concern, because when it is taped into its cast, it will also appear lifted.
Aside from being worried that I would roll onto my face in my sleep, I felt fine. The hospital gave me gauze and tape to apply beneath my nose, and I figured out a way to tape it to the side of my cast, sparing my skin from the adhesive. The hospital had given me a NeilMed nasal rinse, but at times the blockage was so severe that the saltwater would shoot back out the same nostril. Still, I functioned like normal and even interviewed the actor Julia Garner, who thought I sounded like I had the flu.
Cast Removal (1 Week Post-Op)

One week later, with residual bruising that I could cover with concealer, it was time to have my cast removed. At the appointment, Dr. Roostaeian pulled gigantic nasal stents out of my nose that were covered in snot and dried blood. Then I could finally blow my nose, which was a moment I had been dreaming of for a week. I was given my first look — it was definitely swollen but looked cute — and I took my first set of “after” photos. He also taught me to tape my nose in case I wanted to minimize swelling, but he let me know taping is not necessary.
I was nervous at that appointment and tried to delay seeing what was underneath. I heard from friends that seeing their faces in the mirror after surgery was jarring. To be honest, it looked like a normal nose — just not my nose. I was not upset the way they had described, but I definitely wanted the swelling to go down. Though I had been forewarned that while healing, the swollen tip would appear upturned, it still drove me crazy (and I felt like I had a “bulb” on the tip of my nose).

Immediately after my appointment, and still very unsure of how it looked, I took my new nose to Erewhon for my favorite smoothie. Then I headed to a work event where no one could believe that I had just had a nose cast removed.
Healing Week 2
With Dr. Roostaeian’s approval, I also did cryotherapy to promote its healing at Pause Wellness and had a vitamin IV of vitamin C, magnesium, glutathione, and a push of NAD+. I focused a lot on lymphatic drainage massage by going to Lymphatic by Siane for regular massages and got his OK to use the oxygenating and cooling CO2Lift Pro Carboxy Therapy Mask ($100), which I did as often as my budget allowed. In addition to flooding the skin with oxygen to promote healing, the cooling effect of the gel is soothing and anti-inflammatory.
By day 12, I thought my nose looked cute. It was the first time I had seen it in makeup, and it was shocking to me because the light/shadow contour truly was mimicking what I typically used makeup to create. I loved the way it looked straight-on when I smiled because the tip no longer dropped down and widened thanks to its new cartilage support behind it. From the side, the tip still bothered me; although it continues to refine by the day, the swelling is real and will be for four months.

Healing Week 3
My friends tell me that it does not look like I had anything done; that my nose just looks good. But as its owner, I tend to scrutinize it. While I wait out the first four months of the most noticeable swelling, I am amazed by the degree to which its inflammation can fluctuate on a daily basis. I will also say that my nose looked amazing after receiving a Signature Facial by aesthetician Katie Sobelman, with gentle facial and buccal massage, microcurrent, PEMF, and more, topped off by my beloved CO2Lift mask. I run every modality by my surgeon, which is probably very annoying, but he has been a gracious ally in my rigorous healing journey.
I did have a setback in healing at day 19, when I got injections of regenerative Nanofat and PRP in my face. Dr. Roostaeian had approved this procedure — so long as the doctor did not touch my nose — but warned that it might cause swelling due to the injectable delivery method. Suffice it to say, my entire face, including my nose, blew up. This gave me important perspective because the nanofat injections were a much more difficult procedure than my baby rhino. A little over two weeks later, the swelling subsided and the contours of my face started returning to their baseline.
Is Baby Rhinosplasty Worth It?
For me, yes, but that does not mean it is worth it for everyone.
Aesthetically, it resolved my main complaint with my nose when I smiled in photos, and I no longer worry about how it will age. (Board-certified plastic surgeon Marc Mani let me know that nose tips get droopier with age.) But remember that this is a regular stressor for me because of the nature of my job, which requires frequent headshots of makeup and skin care; it simply comes up more often for me than for the average baby rhino-seeker.
As for the septum repair, I will say that arrived on the day of surgery with sinus pain, and I have not had it since. Aside from my first week of healing, I have not woken up unable to breathe through my nose the way I used to, so I have noticed a major improvement in my nasal breathing.
Remember that I also had a remarkably easy recovery; so swift that some have suggested I’m a “super-healer.” I have friends that have had complex rhinoplasties, and I want to make it clear that their recoveries were not as easy as mine. My positive experience has to do with Dr. Roostaeian’s skill and the subtlety of the baby rhinoplasty he performed.
I am now at six weeks post-op. It took me less than two weeks to get used to my nose, even in its swollen state. I already like it more straight-on, although the side view of the healing tip still occasionally irks me six weeks later. Some days I experience worse swelling than others — most recently when my dog hit me in the nose with the surgical cone around her neck — but I have an extensive toolkit of healing modalities to draw from instead of fixating.
Dr. Roostaeian tells me that around month four, my nose will be incredibly close to the end result. Then, for up to a year or even two, continued refinement will take place in the tip, making my result better and better. Now with the surgery behind me, I think it speaks to my confidence in my decision — and my surgeon — that I have referred several of my friends to his practice.
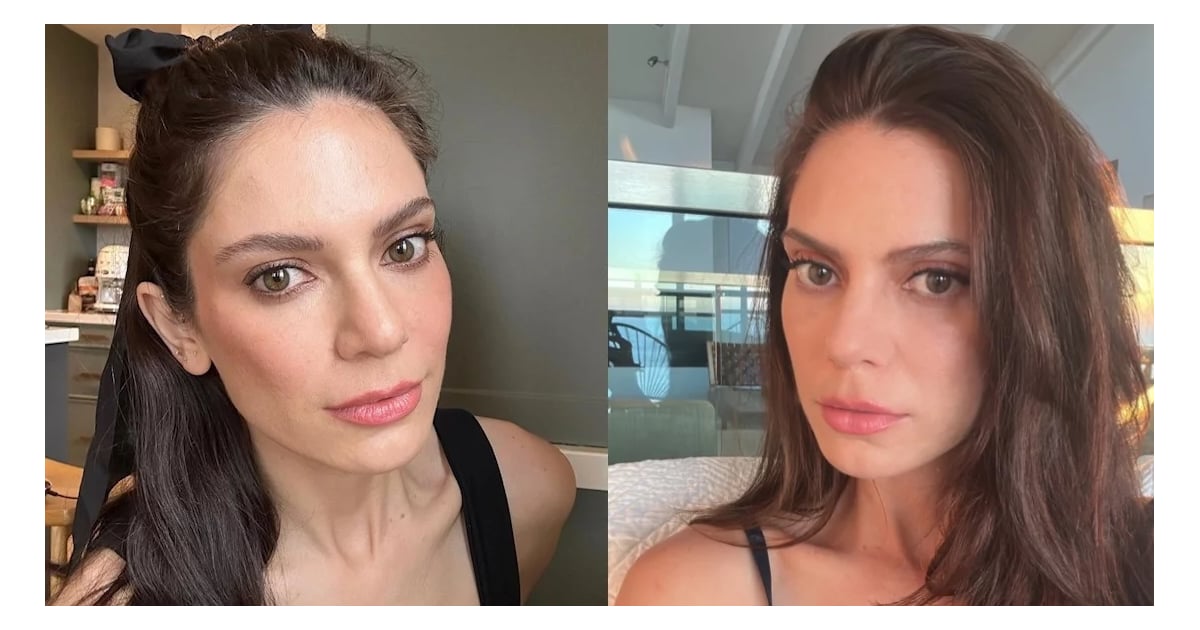
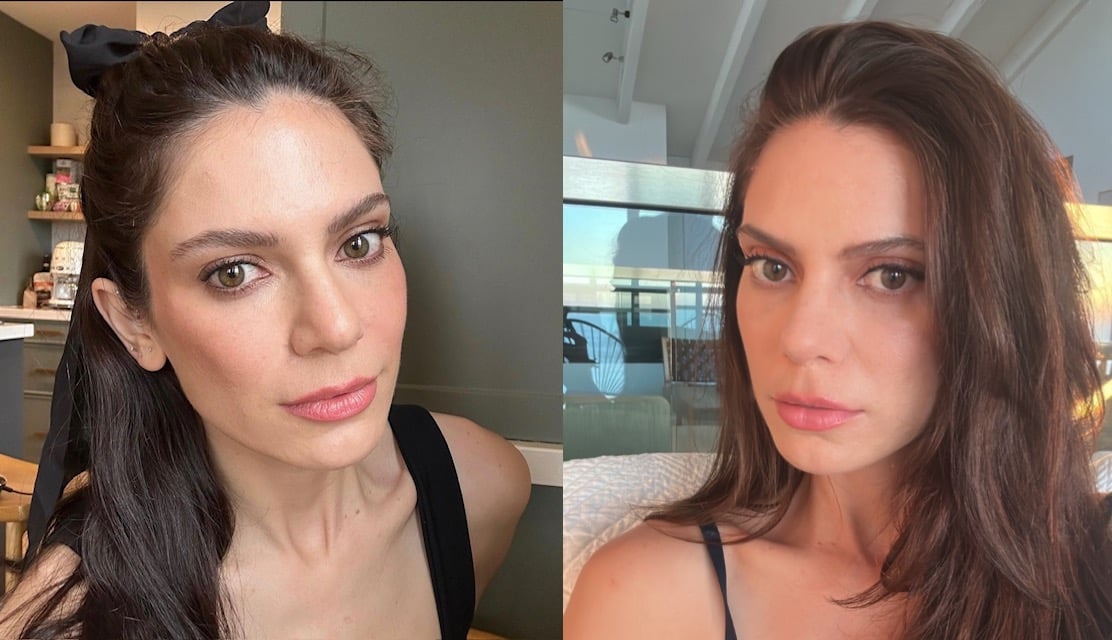
Image Source: Jessica Ourisman